2. Kim KH, You D, Jeong IG, Kwon TW, Cho YM, Hong JH, et al. Type II papillary histology predicts poor outcome in patients with renal cell carcinoma and vena cava thrombus. BJU Int 2012;110(11 Pt B):E673-8.


3. European Association of Urology. EAU Guidelines. Arnhem (Netherlands): European Association of Urology; 2023.
4. Vinzant NJ, Christensen JM, Smith MM, Leibovich BC, Mauermann WJ. Perioperative outcomes for radical nephrectomy and level III-iv inferior vena cava tumor thrombectomy in patients with renal cell carcinoma. J Cardiothorac Vasc Anesth 2022;36(8 Pt B):3093-100.


5. Topaktaş R, Ürkmez A, Tokuç E, Kayar R, Kanberoğlu H, Öztürk Mİ. Surgical management of renal cell carcinoma with associated tumor thrombus extending into the inferior vena cava: a 10-year single-center experience. Turk J Urol 2019;45:345-50.


8. Lue K, Russell CM, Fisher J, Kurian T, Agarwal G, Luchey A, et al. Predictors of postoperative complications in patients who undergo radical nephrectomy and IVC thrombectomy: a large contemporary tertiary center analysis. Clin Genitourin Cancer 2016;14:89-95.


9. Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC Cancer Staging Manual. 8th ed New York: Springer International Publishing; 2017.
10. Blute ML, Leibovich BC, Lohse CM, Cheville JC, Zincke H. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus. BJU Int 2004;94:33-41.


11. Shiff B, Breau RH, Mallick R, Pouliot F, So A, Tanguay S, et al. Prognostic significance of extent of venous tumor thrombus in patients with non-metastatic renal cell carcinoma: results from a Canadian multi-institutional collaborative. Urol Oncol 2021;39:836.e19-836.e27.


12. Klatte T, Pantuck AJ, Riggs SB, Kleid MD, Shuch B, Zomorodian N, et al. Prognostic factors for renal cell carcinoma with tumor thrombus extension. J Urol 2007;178(4 Pt 1):1189-95; discussion 1195.


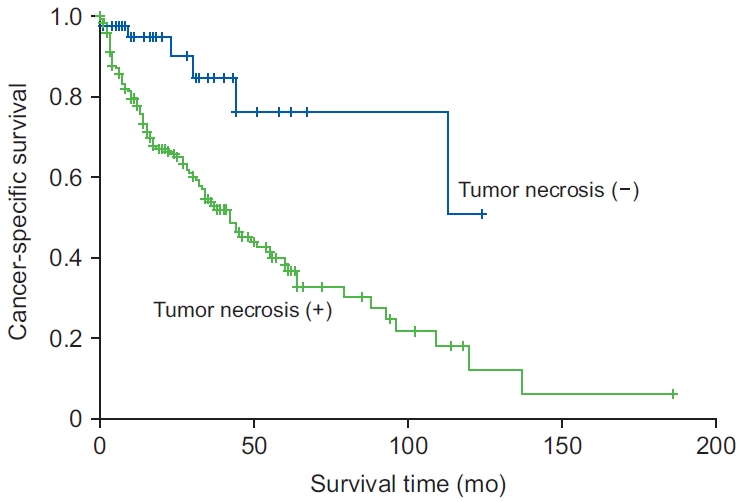
13. Mager R, Daneshmand S, Evans CP, Palou J, Martínez-Salamanca JI, Master VA, et al. Renal cell carcinoma with inferior vena cava involvement: Prognostic effect of tumor thrombus consistency on cancer specific survival. J Surg Oncol 2016;114:764-8.


17. Park JY, Lee JL, Baek S, Eo SH, Go H, Ro JY, et al. Sarcomatoid features, necrosis, and grade are prognostic factors in metastatic clear cell renal cell carcinoma with vascular endothelial growth factor-targeted therapy. Hum Pathol 2014;45:1437-44.


19. Edwards JG, Swinson DE, Jones JL, Muller S, Waller DA, O’Byrne KJ. Tumor necrosis correlates with angiogenesis and is a predictor of poor prognosis in malignant mesothelioma. Chest 2003;124:1916-23.


21. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al., editors. AJCC cancer staging manual. 6th ed. New York: Springer-Verlag; 2002.















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


